Rancho Cucamonga
Rancho Cucamonga
Upland
Glendora
Redlands
- About Us
- Dental Implants
- Oral Surgery Services
- Wisdom Teeth Removal
- Corrective Jaw Surgery
- Bone Grafting
- Facial Trauma
- Anesthesia Services
- Pediatric Oral Surgery
- Impacted Canines
- Oral Pathology
- TMJ Treatment
- Exparel
- MSE, MARPE
- Temporary Anchorage Devices
- PAOO, SFOT
- Obstructive Sleep Apnea (OSA)
- Apicoectomy
- Medication-Related Osteonecrosis of the Jaw
- Frenectomy
- View All Services
- Patient Info
- New Patient Registration
- Patient Forms
- Payments & Insurance
- Video Learning Center
- Informed Consent Videos
- Photo Gallery of Cases
- After Surgery Instructions
- Before Intravenous Anesthesia Sedation
- After Wisdom Tooth Removal
- After Dental Implant Procedure
- After Tooth Extraction or Multiple Extractions
- After Orthognathic or Jaw Corrective Surgery
- After Sinus Lift
- After Socket Bone Grafting
- After Exposure of An Impacted Tooth
- Soft Food Diet Recommendations
- Sinus Precautions
- Prescription Medication Guide and Log
- View All Patient Instructions
- Our Blog
- Reviews
- Referring Doctors
- Contact Us
Blog
Dental implants are one of the most effective options available to restore your smile’s form and function. Whether you are...
There are 2 options for permanently replacing a tooth or multiple teeth: dental implants or a dental bridge. There are...
If you are between the ages of 15 and 21 you will likely require the procedure in the near future....
April 18, 2023
In the past, dentures were traditionally the only tooth replacement option available for anyone missing all of their teeth. Dental...
Oral Surgeons are surgical specialists. Oral Surgeons are specialists who spend 4-6 years of surgical training after dental school through...
February 15, 2023
Impacted or emerging wisdom teeth affect almost everyone. Typically, they begin emerging during adolescence, and if you are a teenager,...
July 19, 2022
Answers to Common Questions About Dental Implants Why select dental implants over other options? What is a dental implant made...
January 1, 2018
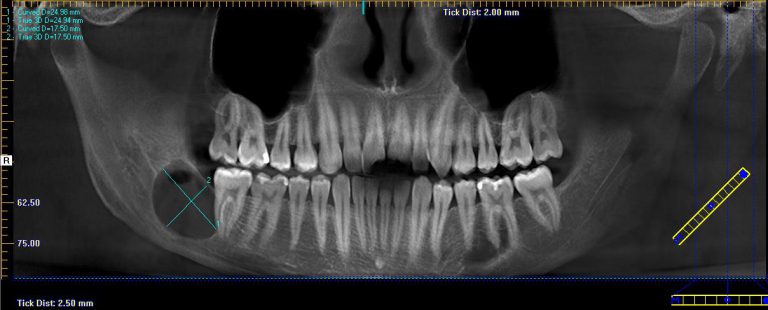
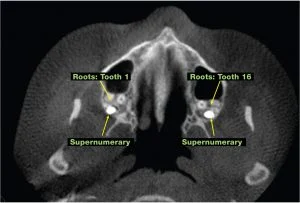
I remember one particularly hot Friday in the office, as I sat down to review some radiographs with a toddler...
August 1, 2017
Hyperdontia is a dental developmental alteration resulting in an increased number of teeth. The occurrence of hyperdontia is between 1% and...