Hyperdontia is a dental developmental alteration resulting in an increased number of teeth. The occurrence of hyperdontia is between 1% and 3.5% in the permanent dentition and 0.3% and 0.6% in the primary dentition, respectively. It is found more commonly in males at a ratio of 2:1. Though the location of the supernumerary teeth may have some variability, the mesiodens, found behind the maxillary central incisors, is the most common, with some studies showing greater than 50% prevalence amongst all hyperdontia patients. The most common location for a supernumerary is the anterior maxilla, followed by the premolar region and, lastly, the wisdom teeth.
Patient #1: 16 y/o female referred for asymptomatic wisdom tooth evaluation. Supernumerary maxillary wisdom teeth incidentally found on CT scan.
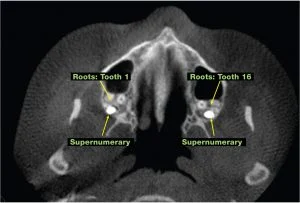

Coronal 3 D CT Scan Posterior view showing location of supernumerary teeth
The two most common syndromes associated with supernumerary teeth are cleidocranial dysplasia and Gardner’s syndrome; these arealso seen in a higher prevalence of patients with cleft lip and palate. The etiology of hyperdontia is unknown, but common theories include genetic and environmental factors and the hyperactivity of the dental lamina theory.
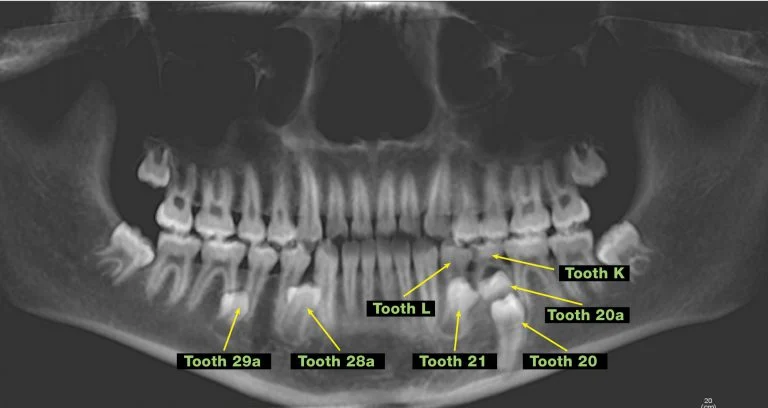
Patient#2: As part of the orthodontic treatment plan, this 14 y/o male referred for removal of mandibular supernumerary teeth. Patient has a history of retained primary teeth K and L with delayed eruption of teeth 20 and 21. Some potential consequences if treatment option is observation: prevention of eruption, cyst formation and damage to adjacent teeth.
The clinical presentation associated with supernumerary teeth can vary from patient to patient. Because only 25% of the supernumerary teeth, specifically the mesodens, erupt into the oral cavity, the majority of the patients are asymptomatic. Clinical findings that raise the index of suspicion of a supernumerary tooth include the following: disruption in the eruption pattern or over-retained teeth, asymmetric eruption pattern, and ectopic eruption of either the primary or permanent dentition. If any these situations should arise, the clinical suspicion for a supernumerary tooth is high; the clinician should proceed with radiographic evaluation with a simple periapical x-ray. Though some of you may remember the SLOB rule radiographic technique to identify position (same lingual, opposite buccal), the cone-beam 3D scan is a more precise method to identify location, pathology, and consequences of possible surgical intervention.
Patient #3: 5 y/o male referred by pediatric dentist for evaluation of right maxillary swelling. Patient recently lost teeth E and F. Clinical exam: right maxillary swelling from right canine to contralateral incisor, missing teeth E and F, and tooth D mobile. CT scan: displaced teeth 7 and 8, 15mm x 15mm x 17mm radiolucent lesion associated with a mesodens. Observation is not an option, surgical intervention is necessary.

The management of supernumerary teeth includes observation or surgical intervention. Common non-surgical complications associated with supernumerary teeth include the following: delayed or prevention of eruption and displacement or rotation of the permanent tooth, including possible diastema formation. Less common sequels of supernumerary teeth include the following: cyst formation, root resorption or dilaceration of the adjacent tooth root, and nasal eruption. Surgical intervention and the timing of the treatment of supernumerary teeth is based on the age of the patient, incidence of any existing current complications, the risk or anticipation of any future complications, and the risk of surgical intervention to the primary or permanent dentition.
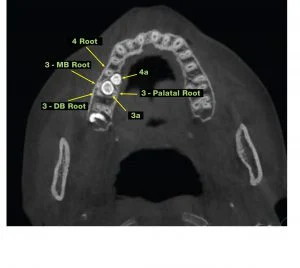
Patient #4: 15 y/o female referred for evaluation and treatment of supernumerary teeth 3a and 4a and extraction of wisdom teeth. Patient instructed to seek consultation after the completion of her orthodontics. Patient is asymptomatic. Possible consequences if surgery is performed: access to the teeth, damage to the root of tooth #3 and sinus communication.








